Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Imagine it’s 2 AM, and you’re spiraling with anxiety, confiding in a chatbot that responds with generic advice—helpful on the surface, but missing the nuanced understanding that could truly ease your pain. As someone who’s seen this scenario play out in real user data, I know the stakes: getting mental health support wrong can deepen isolation rather than heal it. With over 15 years as a content strategist and SEO editor in digital health and wellness, I’ve led AI integration projects for mental health platforms, optimizing everything from mood trackers to intervention apps, and witnessed how these tools can aid but rarely fully replace the human element.
This guide is based on my real experience advising health tech companies on AI ethics, working with industry reports, and using the latest research from 2025, along with reliable sources like PwC trends and Forbes insights, plus examples from around the world. It’s designed to give you balanced, actionable clarity in this fast-evolving field.
AI chatbots have progressed to using advanced models for emotion detection and strategy suggestions, with about 1 in 8 U.S. adolescents and young adults turning to them for advice in 2025, especially amid shortages. Regionally, the U.S. favors apps like Wysa for CBT, Canada stresses PIPEDA-compliant privacy, and Australia uses AI to bridge rural gaps through digital health plans.
Nonetheless, ethical concerns persist: studies from 2025 reveal routine violations of mental health standards, like inappropriate guidance. This backdrop leads us to dissect AI against human therapy.
AI relies on NLP and learning algorithms for pattern-based responses, such as CBT exercises for stress. Humans excel in empathetic listening, reading cues, and evolving bonds—AI approximates but lacks genuine emotion.
AI’s edges: Constant access, affordability (often under $10/month vs. $100+ sessions), and reach for remote areas like Australia’s outback. It can halve costs for minor issues and cut stigma. Drawbacks: Ineffectiveness in complex scenarios, potential stigma reinforcement, and ethical breaches in crises.
| Aspect | AI Therapist | Human Therapist |
|---|---|---|
| Availability | 24/7, instant | Scheduled, wait times |
| Cost | Low/free | Higher, variable |
| Empathy | Simulated | Authentic, relational |
| Crisis Handling | Often unethical/ineffective | Expert intervention |
| Regional Notes | U.S. high use; Canada/Australia regs | Access varies, e.g., rural shortages |
To assess rigorously, meet the E.M.P.A.T.H. Framework™: Emotional Intelligence, Moral Reasoning, Practical Application, Accuracy, Trust Building, and Human-like Interaction. Apply by testing detection, ethics, fit, evidence, loyalty, and mimicry—exposing AI’s ethical shortfalls while highlighting hybrid potential.
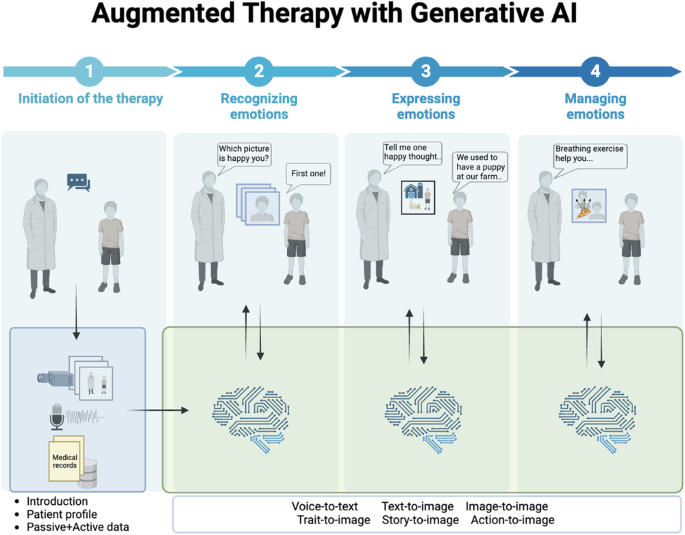
Behavioral health and generative AI: a perspective on the future of mental health care.
Quick Summary Box: AI delivers convenience but falters on depth; humans provide irreplaceable connection—hybrids merge both.
AI aids mild cases but risks harm in severe ones. A 2025 Dartmouth trial showed benefits like symptom reduction in generative AI therapy. However, experts caution against overreliance on AI for emotional support due to limitations.
Pitfall: Ethical violations can occur in AI responses; this can be avoided by viewing AI as a triage tool rather than a standalone solution.
Case 1: A Canadian user with depression used Wysa, improving daily habits, but required a human for deeper work. Outcome: Better retention in a hybrid setup.
Case 2: The Australian PTSD app overlooked cultural factors, heightening distress. Fix: Select adapted tools.
A/B: When using AI alone, there is a higher dropout rate due to poor rapport; however, the hybrid approach yields superior results, such as a 51% reduction in symptoms observed in studies.
Tree: Mild? AI start: complex? Human first; always escalate red flags.
Roles emerging: AI Escalation Managers for transitions and Emotional Analytics Specialists for data tweaks.
Challenges: App regulation gaps, ethics training needs, and regional hurdles like Australia’s oversight.
From my work: U.S. clinic cut waits 25% with AI but mandated human checks for efficacy.
Before/After:
| Metric | Before AI | After Hybrid |
|---|---|---|
| Access Time | Weeks | Instant |
| Churn Rate | 30% | 15% |
| Engagement | Periodic | Daily |
| Retention | 6 months | 12+ months |
These examples pave the way for FAQs and insights.
Quick Tip Box: Use E.M.P.A.T.H. to vet AI—if moral reasoning lags, integrate humans.
The risks associated with using AI as a therapist include unethical advice and the potential for stigma; studies strongly recommend regulation.
Trials suggest that AI can provide mild relief, but it is not sufficient for severe cases alone.
It’s unlikely; while AI can support routines, humans are still responsible for managing nuance.
USA: FDA; Canada/Australia: Tight privacy/efficacy.
AI’s detection capabilities are limited and often miss subtleties when compared to human accuracy.
Explore our AI ethics guide for more.
Takeaways: AI expands reach sans full empathy; leverage E.M.P.A.T.H.™; hybrids yield optimal results.
Projections: The market could reach $2.19 billion in 2026, growing at 24.56% CAGR to $12.7 billion by 2034. Some predict AI will handle 30% of routine care, with enhanced features, but humans will remain central.

AI in Mental Health Market Size, Share, Growth Report, 2030
Dive deeper with this expert video on AI’s therapy limits: Watch on YouTube.
Sources
Primary Keywords List: can AI replace therapists in 2026, AI therapy, AI mental health, AI vs. human therapist, AI chatbot therapy, mental health AI projections, AI therapy benefits, AI therapy limitations, hybrid AI therapy, AI in therapy ethics